In 2021, there were 55 million people worldwide who were living with dementia. And in the next 20 years, this number is expected to double. Dementia is now the 7th leading cause of mortality. And it is among the diseases with the highest costs for society. The most common form of dementia is Alzheimer’s disease (AD), which accounts for about 60 – 80% of all cases.
AD is a neurodegenerative disease. It is the result of progressive damage to the cells and nervous system connections that are necessary for:
- Mobility
- Strength and coordination
- Sensation
- Cognition
However, there is a key area of the brain that remains relatively undamaged in the process. That is musical memory. Music therapy for Alzheimer’s patients can be a powerful tool. Studies have shown that music may improve behavioral issues and reduce agitation which is common during the middle stages of AD.
Even in the late stages, an individual may be able to sing the words to a song from their childhood or tap out the beat. Even after verbal communication has gotten difficult, music provides a method to connect to meaningful moments.
At Shepherd Premier Senior Living in Crystal Lake, Illinois we provide the best in memory care. Keep reading to learn more.
Music Therapy and Active Aging
 Music therapy is one of the types of active aging programs that are offered to elderly individuals with cognitive disabilities such as Alzheimer’s and Dementia. The value of music therapy in the field of memory care is being recognized by the scientific community because studies have reported cognitive, physical, and psychological benefits.
Music therapy is one of the types of active aging programs that are offered to elderly individuals with cognitive disabilities such as Alzheimer’s and Dementia. The value of music therapy in the field of memory care is being recognized by the scientific community because studies have reported cognitive, physical, and psychological benefits.
In one study, forty-two patients with mild to moderate AD experienced music therapy for six weeks. The changes in their results on various neuropsychiatric, anxiety, and depression scales were studied and analyzed. In both mild and moderate cases of AD, the results showed significant improvement in:
- Memory
- Orientation ( the ability to locate yourself in your environment relating to time, place, and people)
- Depression
- Anxiety
In the group with moderate AD, there was also meaningful improvement in:
- Agitation
- Irritability
- Delirium
- Language disorders
The effect on cognitive measures was considerable after only four sessions of music therapy.With the increasing life expectancy, chronic diseases are often seen in elderly people. Currently, no treatment can prevent, stop, or cure Alzheimer’s disease or slow down the neurodegeneration seen in AD and dementia. Treatments used are symptomatic treatments meant to ease the symptoms.
Since the 1960s, psychosocial methods, having to do with the mental, social, emotional, and spiritual effects of the disease have been used with medications in the treatment of AD. One of those psychosocial approaches used is music therapy. Music therapy for Alzheimer’s patients strengthens their coping mechanisms. It also increases their ability to communicate, cognitive functions, and adaptation levels (ability to adapt to new situations) in their environment.
Confirmation continues to mount that regardless of severe impairment of episodic (the ability to recall past experiences), and moderate impairment of semantic memory (the ability to recall words, numbers, or concepts), some patients with AD have a well-preserved memory of musical information. This is evident even in the advanced stages of the disease.
Furthermore, brief exposure to music was shown to have positive effects on recalling episodic memories, even when the music was unrelated to the recalled event. This suggests that musical memory recall can lead to benefits in the realm of both types of memory recall. In addition, there is new evidence that music therapy support can improve standardized scores in patients who have dementia or are at risk for it.Music can also reduce behavioral and psychological conditions such as anxiety and depression in Alzheimer’s patients. A systematic review of non-medication approaches found that music interventions were best at reducing behavioral symptoms in dementia, particularly agitation, and anxiety. One review that collected patients’ saliva before and after music therapy to measure cortisol (often called the stress hormone) levels, showed that music could lower overall stress levels.
AD and the Brain Science of Memory
“Memories are who we are, states Rick Huganir, Ph.D., a researcher studying memory and the director of the Johns Hopkins Department of Neuroscience. “But making memories is also a biological process.” This memory-making process raises many questions such as:
- What is the effect of this process on our brains?
- How do learning and experiences change the connections in our brains and create memories?
The answers may improve memory in people with dementia and new treatments for PTSD.When you learn something, even something as simple as someone’s name, you create connections between neurons in the brain. The places where neurons connect and communicate with each other are called synapses. These synapses create new routes between brain cells–basically remapping your brain.
Brain neurons then use electrical impulses and chemical signals to send information between different areas of the brain, and between the brain and the rest of your nervous system. The massive number of possible connections gives your brain unimaginable flexibility. Each of your brain’s 100 billion nerve cells can have 10,000 connections to other nerve cells.
Depending on how often you’re exposed to an event, those synapses get stronger or weaker. The more often you’re exposed to an activity (like a golfer practicing a swing a thousand times) the stronger the connections and the less you’re exposed, the weaker the connection. This is why it’s so hard to remember someone’s name after the first meeting.Many research questions about memory may have answers in the complicated interactions between certain brain chemicals (mainly glutamate) and neuron receptors. Dr. Huganir discovered that when mice are exposed to traumatic events, the level of neuronal receptors for glutamate increases at synapses in the fear center of the brain. This encodes the fear linked with the memory.
However, when those glutamate receptors are removed, the strength of the connections is reduced. This, essentially, erases the fear element of the trauma but still leaves the memory. New drugs are being developed to target those receptors. The hope is that deactivating the receptors could help people with PTSD by reducing their fear. On the other hand, strengthening them could improve learning, especially in people with cognitive dysfunction or AD.
Ten Early Warning Signs of Alzheimer’s Disease
There is now agreement that Alzheimer’s disease begins with a long phase when there aren’t any recognizable symptoms (asymptomatic). It’s important to recognize the early signs when they do appear.
- Memory loss that upsets daily life
Particularly in the early stage, one of the most common signs of AD is forgetting information that was recently learned. Other signs include:- Forgetting important events or dates
- Repeatedly asking the same questions
- Increasing need to rely on memory aids or family members for things they used to handle on their own
- Difficulties with planning or solving problems
Some people may experience changes in their ability to follow a plan or work with numbers. It’s common to have problems following a recipe or keeping track of monthly expenses. - Trouble completing routine tasks
It’s often difficult for people with AD to complete daily tasks. They may have trouble:- Driving to a familiar place,
- Putting together a grocery list, or
- Remembering the rules of a favorite game.
- Confusion about time and place
People with Alzheimer’s often lose track of dates, seasons, and time passing. If something is not happening immediately, they may have trouble understanding it. They may sometimes forget where they are or how they got there. - Problems understanding visual images and spatial relationships
Having problems with vision is a problem for some people with AD. This can lead to difficulty reading or balancing. Problems judging distance and recognizing colors or contrast can cause problems while driving. - New difficulties with words when speaking or writing
People living with AD may have problems following or joining a conversation. At times they may stop in the middle of a conversation and not be able to continue or they may repeat themselves. There may be struggles with vocabulary or difficulty naming a familiar object. - Losing things and losing the ability to retrace steps
People with Alzheimer’s often put things in unusual places and be unable to go back over their steps to find them. They may accuse other people of stealing. - Poor or decreased judgment
AD patients may experience changes in decision-making skills or poor judgment. It may be when handling money or taking care of their grooming. - Withdrawing from work or social activities
They may have changes in their ability to hold or follow a conversation. This may lead them to withdraw from social activities, hobbies, etc. - Changes in personality and mood
People with Alzheimer’s may experience changes in their mood and personality. When out of their comfort zone, they may become:- Suspicious
- Confused
- Depressed
- Fearful
- Anxious
- Upset with friends
If you recognize one or more of these signs in yourself or someone else, it’s normal to feel uncertain or nervous about talking about these changes. But these are important health concerns that need to be evaluated by a doctor.
Tips for Selecting Music
Here are some tips for selecting songs for music therapy for Alzheimer’s:
- Discover music that’s familiar and enjoyable for the person. If it’s possible, let them choose the music.
- Your source of music shouldn’t be interrupted by commercials–this can confuse you.
- Use the music to create the mood you want. For example, a peaceful piece of music can help encourage a calm environment, but playing a faster-paced song from their childhood may boost their spirit and awaken happy memories.
- Encourage movement like clapping and dancing to amplify the enjoyment.
- Avoid sensory overload. Get rid of competing noises by closing windows and doors and turning off the TV. Be sure the music volume is not too loud.
What is Memory Care?
Memory care is a type of residential long-term care that provides intensive, specialized care for people with memory problems. There are stand-alone memory care facilities and there are also special memory care “neighborhoods” for dementia patients in assisted living facilities, retirement communities, and nursing homes.
Memory care was created to provide a safe, structured environment with established routines to lower stress for patients with AD or dementia. Employees help residents with personal care and provide meals just like employees in an assisted living facility. However, the staff is also specially trained to deal with the unique issues that frequently appear as a result of a person’s dementia or Alzheimer’s. Residents are checked on more often and extra support and structure are provided to help them get through their day.
Is Memory Care at Shepherd Premier the Answer?
Many people with AD can still live on their own during the early stages, especially if there is someone to provide regular in-home support. Still, there may come a time when your loved one needs more support than can be provided at home. These questions will help determine if it’s the right time to move to memory care.
- Is the person becoming unsafe in their home?
- Is the health of the person at risk? (or the health of the caregiver?)
- Are their care needs beyond what I’m able to provide?
- Am I becoming stressed, impatient, or irritable?
- Am I neglecting my work, family, and personal responsibilities?
- Would the structure and social interaction at a care facility help?
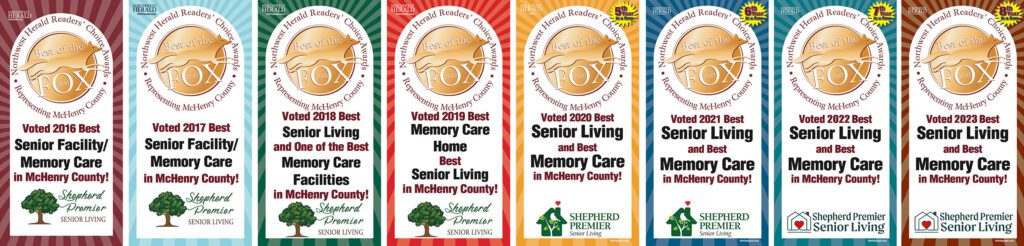
Shepherd Premier Senior Living understands the difficulty of trusting your loved one to the care of someone else. That’s why we serve more than 20 locations in Illinois so your loved one can remain close to you. Although we are large in number, our residential homes have a cozy, intimate atmosphere with a community of 10 to 15 seniors in each one.
If you are questioning whether it’s time to make the move to professional care for your loved one, Shepherd Premier is your answer. Contact us today. Find out why our residents thrive and call our facilities “home”.